What is vocal fold scar?
Scar refers to damage to the vibratory tissues of the vocal fold. Vibration of the lining (epithelium) of the vocal fold depends on the integrity of the layers underneath it, particularly the superficial lamina propria, a loosely-packed network of fibers that functions like a "ball bearing" layer to guarantee that the epithelium on top of it is flexible and not tightly attached to the deeper tissues (see Normal Voice Function). Damage to this layer causes the covering of the vocal fold to be less pliable than it needs to be. Sometimes, scarring is severe enough to cause outright fixation of the epithelium to deeper tissues.
Scar usually results from surgery - and may be unavoidable, as when an invasive cancer must be removed - or it may represent a complication. Scar may also result from damage to the larynx from disease, accident, or severe voice overuse.
A scar is a possible after any surgery of the vocal fold. The probability of scar varies from operation to operation, but is usually small in cases of surgery for benign lesions. The risk of scar, as well as measures to take to prevent scar, should be discussed with your doctor. Most laryngologists agree that quitting smoking, controlling reflux, and not using your voice immediately after surgery are helpful.

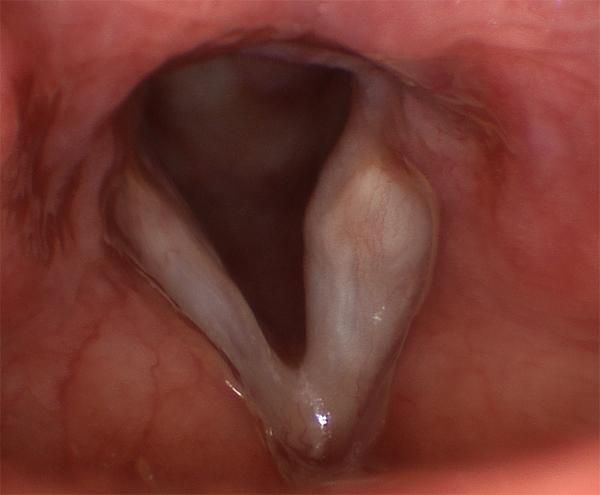
Scar is very difficult to show in still images. The bloodshot, unusually white vocal folds shown here are typical "diffuse scarring" - in this case after sloppy surgery for a pair of vocal fold polyps.
What are the symptoms of vocal fold scar?
Hoarseness results from abnormalities in vibration caused by scarring. The degree of hoarseness is roughly proportional to the extent and severity of the scar. When the mucosa does not vibrate readily, voice production requires more effort, which can result in a strained voice quality, and many people report soreness or tightness of their neck muscles as a result. In general, hoarseness from scarring becomes worse over the course of a day’s voice use, and a little better with voice rest. Scarring does not usually cause difficulty swallowing or breathing.
What does vocal fold scar look like?
Because scarring causes disturbances in vibration, it is usually visible only on stroboscopy. Any laryngoscopy under normal light, whether with a flexible or rigid endoscope, cannot accurately assess scar. For this reason, scar is one of the most often overlooked problems in laryngology.
However, certain features visible on a non-stroboscopic evaluation may suggest scar. These are due to the inflammation and excess deposition of fibrous tissue at the scar site, and include: swelling, redness, and unusually large blood vessels leading into the area - or opacity and dullness of the normally shiny, translucent covering tissue of the vocal fold.
The vocal fold on the left of the image above has a linear scar from an injury caused by the insertion of a breathing tube.

Both vocal folds in this patient have been scarred after more than a dozen surgeries for papilloma.
How is vocal fold scar treated?
Scar is much easier to prevent than to repair, and so every measure must be taken in the way of prevention when planning vocal fold surgery. Before surgery, these include controlling acid reflux and eliminating smoking. After surgery, these include voice rest and appropriate voice therapy to eliminate harmful vocal habits. During microlaryngoscopic surgery, a surgeon must use careful microscopic technique to avoid unnecessary trauma to the superficial lamina propria, and preserve all mucosa covering the vocal fold that is unaffected by the lesion.
The use of lasers for surgery of the vocal fold is a subject of controversy. A majority of otolaryngologists prefer to avoid it. Although the cutting beam is reasonably precise, it appears that the reaction of the vocal fold tissue is somewhat unpredictable, possibly because of the emitted heat. The alternative is microlaryngeal instruments. Although they are more difficult to use, they offer at least equivalent accuracy and less potential for inadvertent damage. Your surgeon will have his or her own opinions on the subject, and it is worth asking about all of these.
Once a scar has developed, it is usually treated nonsurgically, initially. Most scars will improve somewhat with voice therapy and judicious voice use for at least several weeks, until characteristics stabilize over the course of a few examinations. This practice minimizes the amount of tissue that is involved.
Surgical intervention for scar must be considered carefully, for any such intervention stands to make scar worse. The rehabilitation of scarred vocal folds is one of the greatest clinical challenges in laryngology, and investigational efforts continue in a number of areas. To separate the epithelium layer from the tissues to which it is tethered, and replace the damaged “pliability layer” (the superficial lamina propria) between them in order to keep them separated, remains challenging. There is no perfect substitute for superficial lamina propria available, although several groups are working to synthesize such a substance in the laboratory. Surgeons have tried a number of surrogates, including collagen, fat and hyaluronic acid, with varying degrees of success. Often, the damaged tissues re-adhere despite the tissue placed between them - sometimes to a greater extent than before surgery.

